Can you get dental implants if you have bone loss?
People with bone loss can still receive dental implants, but treatment depends on how much bone remains. When there isn’t enough bone for standard implants, options like bone grafting or zygomatic implants, which anchor into the cheekbone, can be used. Zygomatic implants are especially helpful for severe upper-jaw bone loss because they avoid grafting, allow faster recovery, and often enable “teeth-in-a-day” solutions. They have high success rates, but must be placed by very experienced surgeons due to surgical complexity and potential risks. Overall, with proper evaluation and planning, many patients with significant bone loss can still successfully restore chewing function, stability, and quality of life using implant-based solutions.
1. Introduction to Dental Implants with Severe Bone Loss
Based on the zygomatic implant solution for patients with dental implants despite bone loss, several key points simplify the overview. These include assessing remaining bone width and height, evaluating augmentation options for lost bone, and exploring methods to replace teeth while preventing further bone loss. Tooth loss initiates atrophy of the supporting bone, especially in the jaw, altering its structure due to the absence of stimulation from healthy teeth and the interplay of anatomical features. Although most bone loss occurs within the first 18 months, it varies greatly among individuals, presenting unique challenges. Widespread atrophy in the upper jaw may render traditional implant placement impractical, particularly in a one-stage system. In these cases, zygomatic bone implant placement offers a viable alternative, enabling prosthesis attachment to remaining bone. An effective analysis, combined with the clinician’s experience with zygomatic implants, creates pathways for restoring dentition, maintaining bone health, and reestablishing function. After analysis, weighing the pros and cons of each method helps patients choose the option that aligns with their specific needs. (Gaur et al., 2022)(Wakankar et al., 2023)
2. Can you get dental implants with bone loss?

Quick Answer: Yes, you can often still get dental implants with bone loss, but you may need bone-building procedures or alternative implant techniques after a dentist evaluates your remaining bone.
Bone loss is a potential obstacle to receiving dental implants, but patients can often undergo evaluation and find an appropriate solution. The first consideration is to assess available width and height in the area where implants are planned. If bone volume has become inadequate, even when implants seem feasible, it is essential to consider augmentation alternatives, such as bone grafts, membrane barriers, and ridge expansion, which add cost and time to treatment (Gaur et al., 2022). If patients wish to avoid additional procedures, several alternative implant strategies can be discussed, each with specific advantages and risks (Galán Gil et al., 2007).
3. Which Implants for severe bone loss: options and considerations?
Quick Answer: For severe bone loss, zygomatic implants are often used because they anchor into the cheekbone and can avoid bone grafting, but careful evaluation of jaw structure is essential.
Sufficient bone volume is crucial for successful implant placement. Patients with severe bone loss due to chronic tooth loss or tumor resection may need alternatives to standard methods. Zygomatic implants in zygomatic bone allow fixed full-arch rehabilitations in severely resorbed maxillas without bone grafting. Their use needs careful assessment of vertical bone height and circummaxillary anatomy. Severe bone loss often results in diminished vertical dimension of occlusion (VDO). Therefore, evaluating VDO before and after regeneration is vital; maintaining preoperative VDO is ideal. Augmentation techniques like bone grafts or distraction osteogenesis may restore lost VDO but can extend rehabilitation time, even when zygomatic implants could suffice. (Gaur et al., 2022)
4. What are the development, structure, and use of zygomatic implants?
Quick Answer: Zygomatic implants are long implants anchored in the cheekbone, now placed with a less-invasive technique to securely support teeth in patients with severe upper-jaw bone loss.
Zygomatic implants significantly advance prosthetic rehabilitation for severe maxillary atrophy. The placement protocol has shifted from a complex intra-sinus technique to a less invasive extra-sinus procedure, positioning the fixture head on the crestal ridge. The earlier method led to complicated prosthetic designs needing several components. Now, zygomatic fixtures can stabilize maxillary prostheses without natural teeth and with significant bone loss. The zygomatic bone’s dense cortical structure serves as an ideal site for immediate load-bearing implants alongside conventional anterior mandibular implants. A hybrid zygomatic implant has been developed based on literature analysis, enhancing anchorage and reducing mucosal recession during osseointegration. (Aleksandrowicz et al., 2020)(Gaur et al., 2022)
5. How zygomatic implants work in the jaw area
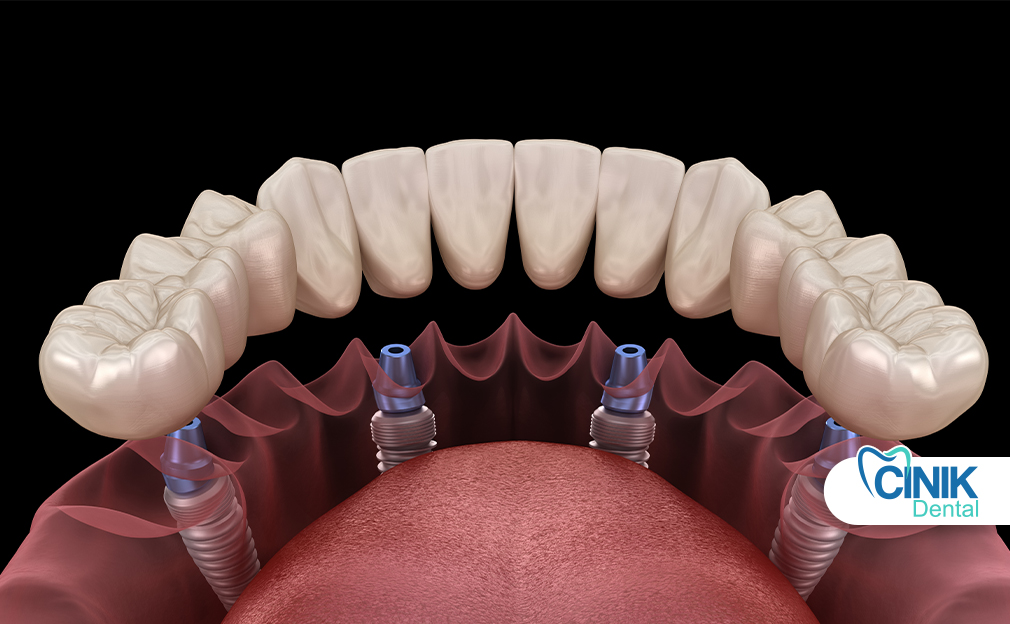
Quick Answer: Zygomatic implants anchor into the cheekbone when the upper jaw lacks bone, providing stable support for teeth even in severe bone loss.
Most jaw areas support dental implants, but some do not, leading to teeth shifting and bite collapse. Zygomatic implants, placed in the cheekbone above the upper jaw, can help avoid these issues when the upper jaw is insufficient. They are long enough to engage abundant, safe bone even in severely resorbed upper jaws. Though less experienced dentists may attempt the procedure, the benefits are notable. The dense, elastic zygomatic bone minimizes stress during placement, reducing fracture or failure risk. Positioned away from the maxillary sinus, it facilitates safe sinus augmentation and grafting. (Galán Gil et al., 2007)
6. What are the functional benefits of using zygomatic implants?
Quick Answer: They give secure support for teeth despite severe upper-jaw bone loss, often allow “teeth in a day,” improve chewing and stability, and reduce the need for bone grafts and long surgeries.
Zygomatic implants provide key functional benefits for prosthetic rehabilitation in areas with bone loss, especially in patients with severe anterior maxilla atrophy. By being anchored in the zygomatic bone, these implants bypass standard sites, eliminating issues like cantilever effects and the need for expensive biomaterials or extensive bone manipulation. They tackle challenges from compromised adjacent teeth and post-extraction bone resorption. Additionally, zygomatic implants can enhance the stability of standard implants in remaining bone. When tailored to specific medical histories and treatment plans, they can offer immediate functional solutions for edentulous maxillae, significantly improving patients’ quality of life. This approach also cuts surgical times by at least fifty minutes compared to alternative methods, reducing costs while enabling quick provisionals or “teeth in a day.”
7. What are the surgical benefits of placing implants in the zygoma?
Quick Answer: They offer a graft-free way to restore teeth in severe upper-jaw bone loss, allow faster, immediate-load treatments, protect key structures, and provide stable support for full-arch restorations.
Zygomatic implants provide a surgical alternative to bone-grafting, particularly for those who have lost teeth in the maxillary region. These implants leverage the zygomatic bone’s intact cortical layer, enabling restoration of lost tooth crowns even with upper maxilla resorption. The implants can be placed using extra-oral or intra-oral techniques, allowing for rapid prosthetic replacements without the need for grafting, thus enhancing both aesthetics and function. They facilitate the re-establishment of occlusion lines and effective bone stimulation within the zygomatic area under fixed, immediately loaded restorations. The implantation process also allows access to the zygomatic region while protecting surrounding anatomical structures. The geographic positioning permits the green stick fracture technique, ensuring accuracy in placement even with challenging panoramic radiograph profiles. Zygomatic implants are ideal for full upper denture reconstructions and crown or bridge restorations, and their incorporation into everyday practice is growing due to advancements by dedicated surgeons. (Galán Gil et al., 2007)(Gaur et al., 2022)
8. Why patients choose Dr. Cinik Dental for zygoma implants

Quick Answer: Patients choose Dr. Cinik Dental for zygoma implants due to the clinic’s expertise, high success rates, minimally invasive methods, and safe management of complex cases.
Patients choose Dr. Cinik Dental for zygoma implants because these implants are an important nongrafting option for functional and esthetic rehabilitation of atrophic maxilla or posterior maxillary defects. Since their introduction, zygoma implants have reduced the number of surgeries and treatment time required for successful rehabilitation. They are indicated when posterior maxillary atrophy exists but adequate anterior bone remains to support conventional implants. The implants range from 30 mm to 52.5 mm, anchoring in the zygoma bone, and are suitable for patients with specific classification patterns. Although beneficial, zygoma implants pose challenges such as difficult surgical access, risk of orbital injury, sinusitis, oroantral fistula, and hematoma.
Patients choose Dr. Cinik Dental for zygoma implants due to the clinic’s expertise in innovative techniques, successful outcomes, and extensive experience with complex cases. Dr. Cinik’s clinic is recognized for precise implantation procedures, including zygomatic implants to rehabilitate severely resorbed maxillae, immediate loading protocols, and methods to prevent complications such as sinusitis. The approach has a proven record of long-term success, addressing challenging anatomical structures with minimally invasive techniques and effective prosthetic solutions (Aleksandrowicz et al., 2020).
9. Which treatment of choice to improve quality of life?
Quick Answer: Zygomatic implants are often chosen to improve quality of life because they restore chewing function and stability in severe upper-jaw bone loss without needing extensive additional implants.
The functional recovery of patients with removable maxillary restorations is directly related to the precision and rehabilitation of the stomatognathic system (Pellegrino et al., 2020). Aiming to support computer-aided rehabilitation of a severely compromised maxilla and ensure improvement in masticatory function with the corresponding psychological benefit, zygomatic implants were utilized. Zygomatic implants, featuring a superior angulation and a long, rigid body in combination with a pre-existing removable denture, were selected as a treatment option to avoid an excessive number of installations and to preclude a transition to a totally implant-supported solution.
10. Frequently asked questions
After a zygomatic implant procedure, patients usually experience minimal swelling from the zygoma, though localized facial swelling may occur at the operation site, peaking between the first and second postoperative days. Most will not need extensive pain management; paracetamol and ibuprofen typically suffice. Patients can resume daily activities within three days but should avoid heavy exercise for one month. Stitches are removed 7 to 10 days post-surgery. While some may return to work sooner, a full week off is recommended. The success of zygomatic implants in extensive atrophic maxilla cases has improved, and thorough patient evaluation before surgery is vital, highlighting advantages over alternatives. These implants are ideal for those with prior graft failures or congenital deficiencies. (Al-Nawas et al., 2023)
10.1. What is the success rate of zygoma implants?
Zygomatic implants show high success rates across studies. In a review of 28 patients with a two-stage zygomatic protocol, the implant success rate was 88.1% over 2 to 8 years, consistent with other studies reporting 95–96% success. Overall survival rates for zygomatic implants are 96.3%, with no major complications. (Galán Gil et al., 2007)
10.2. How long is the recovery period for zygoma implants?
Zygomatic implants can accelerate the rehabilitation process in the severely resorbed maxilla and help patients avoid prolonged periods without teeth or waiting for bone regeneration procedures (Gaur et al., 2022). Immediately after surgery, patients receive provisional prostheses supported by zygomatic implants, which they use for 6 months while the submerged anterior implants integrate. Definitive prostheses can be placed after the zygomatic-implant-supported, or in certain cases, screw-retained, provisional phase.
10.3. Will my face look different after zygomatic implants?
Extensive bone resorption in the maxillary area results in critical defects, limiting conventional implant-supported prostheses for edentulous patients. Zygomatic implants offer an alternative for single or multiple maxillary rehabilitations. These elongated implants are anchored in the zygomatic bone, positioned para-sinus to support immediate or delayed prostheses. While several authors have discussed zygomatic implants effectively addressing atrophied maxilla challenges with high success rates. Techniques encompass zygomatic implant selection, site preparation, positioning, stabilization, suturing, and post-operative protocols. These advancements position zygomatic implants as a reliable solution for atrophied maxilla rehabilitation.
11. Conclusion
Dental implants are a reliable treatment for restoring lost stomatognathic structures, though the posterior maxilla has a low success rate for osseointegration, particularly in previously grafted bone. The aim of treatment is to be minimally traumatic, efficient, cost-effective, and to reduce complications like grafting and postoperative pain. Immediate functional rehabilitation is preferred, utilizing support from cortical and buttress bone. Intraosseous implants have evolved from the Formiggini screw to single-piece implants that support immediate loading. Zygomatic implants offer an alternative for rehabilitating atrophic maxilla cases or when additional anchorage for prostheses is needed, helping to avoid cantilever issues and allowing immediate loading without grafting. They are economically beneficial, minimally invasive, and reduce the risk of complications. Designed for stable retention in patients with severe maxillary bone resorption or post-maxillectomy, zygomatic implants are indicated when conventional implants or grafting are not suitable. Indications for placement include severe posterior maxillary resorption, failure of previous implants, and patient refusal of grafting. Despite surgical risks, their use is increasing due to high survival rates, with the decision to use them relying on factors like bone resorption severity and advancements in conventional implant technology. (Gaur et al., 2022)(Al-Nawas et al., 2023)
References:
Gaur, V., Gala Doshi, A., and Palka, L. “Zygomatic approach with single-piece implants: A technical note.” 2022. ncbi.nlm.nih.gov
Wakankar, J., B Mangalekar, S., Kamble, P., Gorwade, N., Vijapure, S., and Vhanmane, P. “Comparative Evaluation of the Crestal Bone Level Around Pre- and Post-loaded Immediate Endoosseous Implants Using Cone-Beam Computed Tomography: A Clinico-Radiographic Study.” 2023. ncbi.nlm.nih.gov
Galán Gil, S., Peñarrocha Diago, M., Balaguer Martínez, J., and Martí Bowen, E. “Rehabilitation of severely resorbed maxillae with zygomatic implants : an update.” 2007. [PDF]
Aleksandrowicz, P., Kusa‐Podkańska, M., Tomkiewicz, W., Kotuła, L., Perek, J., and Wysokińska‐Miszczuk, J. “Platform switch hybrid zygoma implants improve prosthetics and marginal bone protection after extra‐sinus placement.” 2020. ncbi.nlm.nih.gov
Pellegrino, G., Basile, F., Relics, D., Ferri, A., Grande, F., Tarsitano, A., and Marchetti, C. “Computer-Aided Rehabilitation Supported by Zygomatic Implants: A Cohort Study Comparing Atrophic with Oncologic Patients after Five Years of Follow-Up.” 2020. ncbi.nlm.nih.gov
Al-Nawas, B., Aghaloo, T., Aparicio, C., Bedrossian, E., Brecht, L., Brennand-Roper, M., Chow, J., Davó, R., Fan, S., Jung, R., W. Kämmerer, P., V. Kumar, V., Lin, W. S., Malevez, C., Morton, D., Pijpe, J., D. Polido, W., M. Raghoebar, G., J. Stumpel, L., J. Tuminelli, F., Verdino, J. B., Vissink, A., Wu, Y., and Zarrine, S. “ITI consensus report on zygomatic implants: indications, evaluation of surgical techniques and long-term treatment outcomes.” 2023. ncbi.nlm.nih.gov




Leave a Reply